Can Immune Issues Cause Infertility?

Among the many causes of infertility, immune-related factors have emerged as a critical area requiring attention. While most people associate infertility with reproductive organ issues or age-related factors in either men or women, genetic incompatibility between partners can also trigger immune-related infertility. Clinically, some patients who have experienced multiple IVF failures due to immune issues eventually turn to surrogacy. So, can infertility caused by immune factors be resolved through IVF technology?
Can Immune Disorders Cause Infertility?
Yes! When the immune system is not functioning properly, it may mistakenly attack healthy tissues or cells in the body, including embryos. For example, certain antibodies can attack platelets, leading to blood clots that block the blood vessels in the placenta, preventing the embryo from receiving adequate nutrients. This can result in infertility or miscarriage.
A successful pregnancy requires the body’s immune system to be in a state of "immune tolerance," meaning the immune system must tolerate the presence of the embryo. However, if the immune system becomes overactive and produces anti-sperm, anti-endometrial, or anti-egg antibodies, it can make conception very difficult and even lead to recurrent miscarriages.
Causes of Immune-Related Infertility
Immune-related infertility is primarily caused by an imbalance in the immune system, which can be triggered by various factors such as aging, stress, irregular lifestyle, environmental pollution, and even genetics. These factors may cause the immune system to react abnormally, producing antibodies that attack the body’s own cells. Common causes and types of antibodies related to immune infertility include:
-
Anti-Sperm Antibodies: A woman’s body may produce antibodies against sperm, preventing sperm from successfully fertilizing the egg, thus impacting conception.
-
Anti-Endometrial Antibodies: These antibodies can attack the embryo and interfere with its implantation in the uterus, potentially leading to early miscarriage or implantation failure.
-
Antiphospholipid Antibodies (APS): These antibodies increase blood clotting tendencies, leading to blood clots that can cause recurrent miscarriages, delayed fetal development, or even stillbirth.
If you're concerned that immune issues might be affecting your fertility, a blood test can help identify the problem. It is recommended that patients with unexplained infertility, advanced maternal age, premature ovarian failure, recurrent miscarriages, or multiple failed IVF implantations undergo the following immune tests to pinpoint the cause.
What Tests Should Be Done for Immune-Related Infertility?
Immune problems are a significant factor in infertility and miscarriage. To determine if there is an immune issue, blood tests are commonly used. Below are some of the main types of immune tests:
-
Autoimmune Testing: This includes tests for thyroid antibodies, antinuclear antibodies (ANA), and antibodies related to lupus and other autoimmune disorders.
-
Antiphospholipid Syndrome (APS) Testing: This test screens for antibodies linked to recurrent miscarriage and fetal development issues, such as anticardiolipin antibodies and beta-2 glycoprotein antibodies.
-
Thrombosis-Related Testing: These tests assess blood clotting factors and the risk of thrombosis, including D-dimer, Protein S, and Protein C levels.
-
Thyroid Function Testing: Tests for thyroid conditions, such as Hashimoto's thyroiditis and Graves' disease, that may affect fertility.
-
Anti-Sperm Antibody Testing: This test checks for antibodies against sperm that can impair sperm motility and the fertilization process.
Treatment Options for Immune-Related Infertility
There are several treatment approaches for immune-related infertility. Below are some of the common methods:
Immunosuppressive Therapy
If infertility is caused by an autoimmune disorder, doctors may use immunosuppressants to control the immune response and help the embryo implant successfully.
Intravenous Immunoglobulin (IVIG) Therapy
This treatment involves administering immunoglobulin intravenously to regulate the immune system, reducing the chances of the embryo being attacked by the immune system.
Anticoagulant Therapy
For patients with antiphospholipid antibodies, doctors may prescribe anticoagulants such as heparin to reduce the risk of blood clots and support healthy fetal development.
Third-Generation IVF Technology (PGS/PGD)
At RSMC in the U.S., third-generation IVF technology is used for immune-related infertility cases. Preimplantation Genetic Screening (PGS) or Diagnosis (PGD) is performed to select healthy embryos before implantation, reducing the risk of immune reactions and increasing the chances of a successful pregnancy.
Surrogacy
If a woman is unable to carry a pregnancy due to immune issues, surrogacy is an option. The surrogate’s uterus provides a safer environment, allowing the embryo to develop without being affected by the intended mother’s immune system.
Further Reading:

RSMC is Committed to Making Your Dream of Building a Family Come True
The United States leads the world in IVF technology and pregnancy success rates, and California, where RSMC is located, has the most progressive fertility policies. Whether you are single or a same-sex couple seeking IVF with sperm donation, California offers advanced IVF technology and comprehensive legal protections for parentage. RSMC boasts the largest CPA-certified lab in Southern California, providing the best possible environment for embryo development. With over 30 years of clinical experience, we help overcome immune-related infertility, whether through self-pregnancy or surrogacy. We are confident in our ability to help you achieve your dream of having a child.
If you would like to learn more about the process and costs, or schedule a free online consultation with our U.S. medical director, please contact our multilingual team available 24/7 via: Line / WeChat: rsmctw, Whatsapp: +1 858-342-6046.
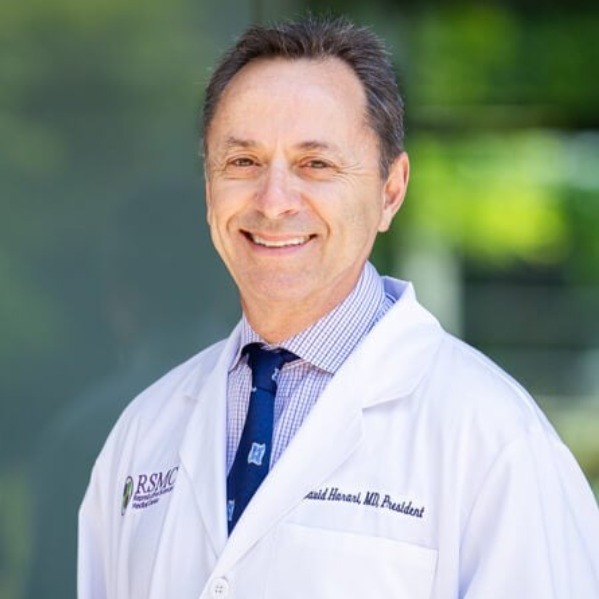
Physician Information
DR. DAVID HARARI | Medical Director & President of RSMC Medical Group
Dr. David Harari earned his medical degree from the University of Georgia Medical Center. He completed his internship at the Medical College of Georgia and subsequently underwent residency training at Mercy Hospital Medical Center. With over 30 years of clinical experience, Dr. Harari currently serves as the President of the San Diego Obstetrical and Gynecological Society, an association with more than 400 professional OB-GYN physician members.In his practice, Dr. Harari places great emphasis on respecting each patient's individual preferences and providing them with the most professional treatment plans. He works collaboratively with his patients to help them achieve their goals. Dr. Harari strongly believes in the importance of clear communication and understanding between doctor and patient. He is always willing to share his extensive medical experience and offer the most professional medical advice.
About Dr. David Harari
Other
-
2024/11/18ivf
What is a Uterine Polyp? Does It Affect Fertility?



