What is a Uterine Polyp? Does It Affect Fertility?
The term "uterine polyp" is not unfamiliar to many women. However, any health issue related to the uterus often causes concern, particularly when it comes to its potential impact on fertility. In fact, uterine polyps are a common type of proliferative change within the uterus, though their exact cause is still not fully understood. Research suggests that hormones—especially estrogen—play a significant role in the growth of these polyps. So, what exactly is a uterine polyp, and does it really affect fertility? Let's delve into this common yet often misunderstood condition.

What is a Uterine Polyp?
A uterine polyp is a growth attached to the inner wall of the uterus, extending into the uterine cavity. These polyps are typically formed due to excessive growth of the endometrial cells, and are also known as "endometrial polyps." Studies show that fluctuations in estrogen levels may stimulate the overgrowth of endometrial cells, leading to the formation of polyps. Most uterine polyps are benign, but some may develop into precancerous lesions. The size of these polyps can vary widely, from just a few millimeters (about the size of a sesame seed) to several centimeters (about the size of a golf ball). Polyps can occur singly or in multiples. They are connected to the uterine wall either by a broad base or a thin stalk. While more common in women approaching or past menopause, uterine polyps can also occur in younger women.
Symptoms of Uterine Polyps
Many people with uterine polyps have no symptoms at all. They may only be discovered during a routine ultrasound or through a hysteroscopy if the patient is undergoing fertility treatments. However, not everyone is asymptomatic. If you experience any of the following symptoms, it may indicate the presence of uterine or cervical polyps, and it's recommended to seek medical advice for further evaluation:
-
Unexpected bleeding between periods
-
Prolonged menstrual periods
-
Heavy or abnormal menstrual bleeding
-
Infertility
Additionally, some younger patients may report light spotting or bleeding before their period. If you experience this, it could be due to a uterine polyp or another underlying issue, so it's important to get checked by a healthcare professional.
If you are experiencing any of these symptoms, try not to worry too much! Around 10% to 24% of women may develop uterine polyps at some point in their lives, with the highest incidence occurring between the ages of 40 and 50. Many women with uterine polyps have no obvious symptoms, and these polyps are often discovered incidentally during routine exams or infertility investigations. However, some women may experience irregular bleeding outside of their menstrual cycle, excessive menstrual bleeding, or extended periods. These symptoms are often caused by the pressure polyps place on the uterine lining, especially under the influence of fluctuating estrogen levels, which can lead to abnormal bleeding.
Furthermore, uterine polyps can impact fertility, especially if the size or location of the polyp interferes with embryo implantation. This can cause issues with conception. Young women may also experience light spotting before their period, which is not always caused by uterine polyps, but it's important to have a gynecological check-up to rule out other potential causes.

Diagnosis of Uterine Polyps
Uterine polyps are often discovered incidentally during gynecological exams, especially through ultrasound or hysteroscopy. Below are some common diagnostic methods:
-
Ultrasound Examination: Ultrasound is a common tool for the initial diagnosis of uterine polyps. It can show abnormal thickening or protruding structures in the endometrium, helping doctors assess the condition of the uterus. However, it can sometimes be difficult to clearly distinguish the size and location of the polyps.
-
Hysteroscopy: Hysteroscopy is a more accurate method where a small camera is inserted through the cervix into the uterine cavity. This allows doctors to directly observe the position, size, and number of polyps, and in some cases, they can be removed immediately during the procedure.
-
Magnetic Resonance Imaging (MRI): In more complex cases, doctors may opt for MRI to get a more comprehensive view of the uterine condition and to rule out other possible abnormalities.
With these diagnostic methods, doctors can more accurately assess the nature of the polyps and develop an appropriate treatment plan, reducing unnecessary health risks.
Impact of Uterine Polyps on Fertility
The presence of uterine polyps can have a certain impact on fertility, particularly when the size or location of the polyps obstructs the implantation of a fertilized egg. Studies show that approximately 15% to 32% of women with infertility may have an association with uterine polyps. Here’s how polyps may affect fertility:
-
Obstruction of Implantation: When polyps are located in key areas of the uterine cavity or cervix, they may prevent the fertilized egg from implanting properly, thereby affecting natural conception.
-
Increased Risk of Miscarriage: The presence of polyps can create an unstable uterine environment, making it difficult for the embryo to develop in the early stages, which increases the likelihood of miscarriage.
-
Reduced Success Rates in IVF: Research indicates that the presence of uterine polyps may decrease the success rate of embryo implantation during in vitro fertilization (IVF), particularly if the polyps are near the implantation area.
For women planning to conceive, removing uterine polyps through surgery can significantly improve the chances of pregnancy. Especially for those considering IVF, polyp removal can be an effective treatment to improve success rates and reduce the risk of treatment failure.
How to Treat Uterine Polyps?
The treatment of uterine polyps depends on the patient's age, the severity of symptoms, and fertility plans. Common treatment options include:
-
Watchful Waiting: If the polyps are small and asymptomatic, doctors may recommend a wait-and-see approach, with regular monitoring to ensure the polyps do not grow or develop any abnormal changes.
-
Hysteroscopic Polypectomy: For patients with irregular bleeding or those planning to conceive, hysteroscopic polypectomy is a common minimally invasive surgical procedure. This method allows for the direct removal of the polyps and is usually performed on an outpatient basis with a short recovery time, making it suitable for most patients.
-
Medications: In certain cases, doctors may recommend hormone-based medications to control the growth of the polyps, particularly for postmenopausal women. This treatment can reduce bleeding symptoms, but its effects are typically temporary, and the polyps may recur once the medication is discontinued.
-
Hysterectomy: For patients with recurrent polyps and severe symptoms, especially for postmenopausal women who no longer wish to have children, a hysterectomy (removal of the uterus) may be considered as a last resort to completely address the issue of polyps.
The appropriate treatment should be determined based on the doctor's recommendations, especially for patients with fertility concerns. Minimally invasive surgery is often the preferred option for those wishing to preserve fertility, as it helps maintain a stable uterine environment. Regular post-surgery follow-ups are also important to minimize the risk of recurrence and ensure long-term health.
RSMC Helps Make Your Family Dreams Come True
The United States leads the world in IVF technology and pregnancy rates, and California, where RSMC is located, has some of the most progressive fertility policies. Whether you're single or a same-sex couple using sperm donation, we offer advanced IVF technology with robust legal protections for parental rights.
RSMC has the largest IVF laboratory in Southern California, certified by the national CPA. With over 30 years of clinical experience, we are confident in our ability to help you achieve your dream of parenthood, whether through traditional conception or surrogacy.
If you'd like to learn more about the process, costs, or schedule a free online consultation with our medical director in the U.S., please contact our multilingual team with no time zone barriers via:Line / WeChat: rsmctw,WhatsApp: +1 858-342-6046.
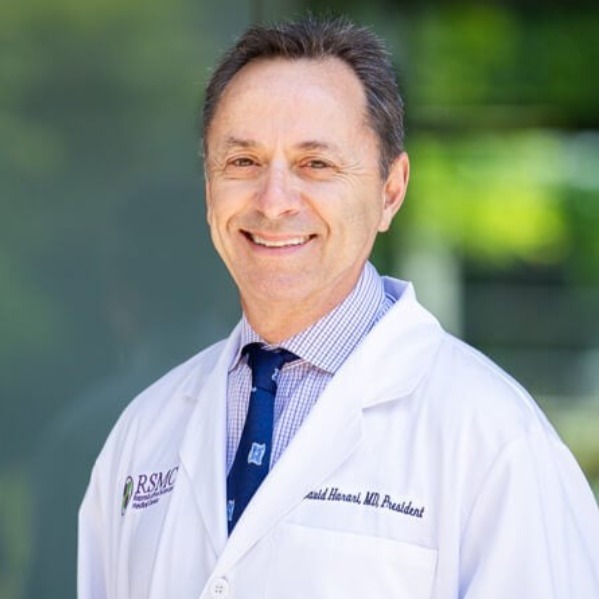
DR. DAVID HARARI
Medical Director of RSMC San Diego
Dr. Harari earned his Medical Doctorate from the University of Georgia Medical Center, completed his internship at the Georgia Medical School, and later finished his residency training at Mercy Medical Center. With over 30 years of clinical experience, Dr. Harari is currently the President of the San Diego Obstetrical and Gynecological Society, which boasts over 400 professional OB-GYN members. Throughout his practice, Dr. Harari deeply respects each patient's personal wishes, providing them with the most professional treatment plans and working collaboratively to help them achieve their goals. He believes in the importance of clear communication and mutual understanding between doctors and patients and is always eager to share his extensive medical experience and offer the best professional advice.
About Dr. David Harari
Other
-
2024/11/06ivf
How to Optimize Egg Quality for IVF at an Advanced Age?



