A Must-Read for Expectant Mothers: All About Down Syndrome Screening!
Down syndrome screening is one of the essential tests for many pregnant women during pregnancy. This screening helps expectant parents understand the risk of their baby having Down syndrome, providing guidance for subsequent pregnancy management. Since Down syndrome can have long-term effects on a child’s physical and mental development, early screening and intervention are particularly important.
Typically, Down syndrome screening is conducted between the 10th and 13th weeks of pregnancy. If early screening is missed, a second stage of screening can still be performed during the mid-pregnancy period. However, if the results indicate a high risk and the pregnancy is terminated at a later stage, the fetus is more developed, and surgical risks, such as bleeding, infection, or uterine damage, may increase.
Therefore, it is highly recommended for pregnant women to schedule Down syndrome screening early to safeguard both maternal and fetal health.

What Is Down Syndrome?
Down syndrome, also known as Trisomy 21, is a genetic chromosomal disorder caused by an abnormality in the 21st chromosome. It significantly impacts the intellectual development, physical appearance, and growth process of affected individuals. While the exact cause of Down syndrome remains unclear, studies show that the risk of having a baby with Down syndrome increases significantly with maternal age, especially in women over 35. The incidence of Down syndrome in newborns is approximately 1 in 700 to 1 in 1,000, but the risk is much higher among older mothers.
Based on variations in chromosomal abnormalities, Down syndrome is categorized into three types:
-
Standard Type (Nondisjunction): This accounts for about 95% of cases, where each cell contains an extra full copy of chromosome 21.
-
Translocation Type: Representing around 4% of cases, this occurs when chromosome 21 attaches to another chromosome, often involving a hereditary component.
-
Mosaic Type: The rarest form, making up about 1% of cases, where only some cells have the extra chromosome 21, potentially resulting in milder symptoms.
Common characteristics of individuals with Down syndrome include intellectual disabilities, distinct facial features (such as a flat nasal bridge, wide-set eyes, and upward-slanting eyelids), delayed physical development, and various congenital anomalies such as heart defects and gastrointestinal malformations. Additionally, they are more susceptible to health issues like congenital hypothyroidism, acute leukemia, and infectious diseases, requiring ongoing medical care and intervention.
Screening to assess the chromosomal health of the fetus enables families to make informed decisions during pregnancy and prepare for potential outcomes effectively.
Why Should You Undergo Down Syndrome Screening?
Down syndrome screening allows expectant parents to assess the risk of their baby being affected, enabling better preparation during early pregnancy. Approximately 60% of fetuses with Down syndrome naturally miscarry during early pregnancy. Those who survive often face significant intellectual disabilities, distinct facial features, and multiple congenital anomalies, such as heart defects and gastrointestinal issues. For this reason, many countries have incorporated Down syndrome screening into routine prenatal care. The goal is to reduce potential family burdens, promote healthy childbirth, and improve overall population health.
Early screening enables risk assessment during the initial stages of fetal development. If results indicate high risk, parents can opt for further diagnostic testing, reducing the need for later-term termination and the associated risks to the mother. Therefore, Down syndrome screening is not just a health check but a vital step in protecting family well-being.

What Tests Can Detect Down Syndrome?
Down syndrome screening methods vary based on the stage of pregnancy, ranging from non-invasive initial screenings to more accurate diagnostic tests. Here are the key screening steps and methods:
Early Screening (10–13 Weeks)
During the first trimester, non-invasive blood tests evaluate the risk of Down syndrome. These tests measure two biomarkers: pregnancy-associated plasma protein-A (PAPP-A) and free beta-human chorionic gonadotropin (β-hCG). Combined with factors like maternal age, weight, and gestational age, the results calculate the risk of chromosomal abnormalities. Early screening provides valuable insights into fetal health at an earlier stage.
Mid-Trimester Screening (15–20 Weeks)
Second-trimester screening, often called the "triple or quadruple test," analyzes maternal blood for markers such as alpha-fetoprotein (AFP), human chorionic gonadotropin (hCG), and unconjugated estriol (uE3). These results offer further insights into the likelihood of Down syndrome and help determine whether additional diagnostic tests are needed.
Non-Invasive Prenatal Testing (NIPT)
NIPT is a highly sensitive blood test that analyzes fetal DNA circulating in the mother’s blood to detect chromosomal abnormalities. Conducted as early as 10 weeks into pregnancy, NIPT is highly accurate, non-invasive, and suitable for women of all ages, especially those of advanced maternal age.
By utilizing these screening and diagnostic methods, expectant parents can gain critical information about the chromosomal health of their baby at various stages of pregnancy, enabling them to make informed decisions about prenatal care.
When Is Further Testing Needed?
Current Down syndrome screening involves analyzing the concentrations of alpha-fetoprotein (AFP) and beta-human chorionic gonadotropin (β-hCG) in the mother’s blood, combined with the mother’s age, to calculate and assess risk. AFP levels within the normal range are typically 0.7–2.5 MOM, while higher β-hCG levels indicate an increased likelihood of Down syndrome. If the screening results suggest a higher risk, further diagnostic tests such as amniocentesis or chorionic villus sampling (CVS) are recommended to confirm the findings.
If early or mid-pregnancy screening results show a high risk of Down syndrome, doctors usually advise undergoing one of the following diagnostic tests:
Amniocentesis
Typically performed between the 15th and 20th weeks of pregnancy, this procedure involves using a fine needle to extract a small sample of amniotic fluid through the abdomen for chromosomal analysis. Amniocentesis is highly accurate but invasive, carrying a very low risk of miscarriage. It is usually recommended when screening results indicate a high risk.
Chorionic Villus Sampling (CVS)
Conducted between the 11th and 14th weeks of pregnancy, CVS involves collecting a sample of placental tissue to analyze the baby’s chromosomes. This test provides an earlier diagnosis of chromosomal abnormalities but also carries a slight risk of complications. It should be considered carefully under the guidance of a healthcare provider.
Further Reading:Is Amniocentesis Required for Surrogacy?
Treatment Options for Down Syndrome
Currently, there is no specific cure for Down syndrome. Treatment primarily focuses on early intervention through rehabilitation training and education to improve the quality of life for affected individuals. Close collaboration between medical teams and families is crucial for the growth and development of children with Down syndrome. With consistent support and training, children can make progress in life skills, learning abilities, and social interactions, enabling them to achieve greater independence in daily life.
For prospective parents, Preimplantation Genetic Testing for Aneuploidies (PGT-A) in third-generation IVF technology offers an option for reducing the risk of Down syndrome. This technique screens embryos at the chromosomal level, ensuring only chromosomally normal embryos are implanted, significantly lowering the likelihood of chromosomal abnormalities. In the U.S., PGT-A also allows for legal gender selection. This approach is particularly beneficial for those with a family history of genetic conditions or older mothers, providing higher safety and success rates for healthy pregnancies.

RSMC: Comprehensive PGT-A Testing for Successful Parenthood
At RSMC, all IVF treatments include PGT-A screening, and surrogacy programs strictly implant only high-quality embryos confirmed as chromosomally normal through PGT-A. Additionally, RSMC implements five rigorous prenatal tests to ensure the health of both the surrogate mother and the future child:
-
Early pregnancy blood screening
-
Non-Invasive Prenatal Testing (NIPT)
-
Nuchal Translucency (NT) ultrasound
-
Quadruple screening test
-
Fetal echocardiography
These tests help detect and manage potential risks early, safeguarding the well-being of the surrogate mother and the baby.
Why Choose RSMC for IVF in the U.S.?
In addition to gender selection, RSMC provides IVF services for same-sex couples and single individuals and offers surrogacy options for those unable to carry a pregnancy. After PGT-A testing, our physicians will discuss embryo quality and confirm the selected embryo’s gender before implantation.
RSMC’s lab is among the few globally certified at the 7.5-day embryo culture level and holds dual accreditation from the College of American Pathologists (CAP) and the Clinical Laboratory Improvement Amendments (CLIA)—the highest international standards for laboratories.
Given that medical treatments are highly personalized, RSMC begins with a detailed review of your medical history. Once we’ve gathered the necessary reports, a free online consultation with our U.S.-based medical director will be arranged. Whether you’re pursuing self-egg/sperm IVF, donor-assisted IVF, or third-party surrogacy, RSMC has over 30 years of expertise, supported by top fertility specialists, one of North America’s largest egg banks and surrogacy networks, comprehensive insurance coverage, and legal experts managing all documentation for your baby’s birth.
From the initial consultation to the baby’s arrival, our professional team handles every detail to ensure a seamless experience.
If you're interested in our programs, we invite you to schedule a free online consultation with our 24/7 multilingual support team.Contact us via Line / WeChat: rsmctw,WhatsApp: +1 858-342-6046 .
Further Reading:The Ultimate Guaranteed Success Plan: 80% Refund if Unsuccessful!
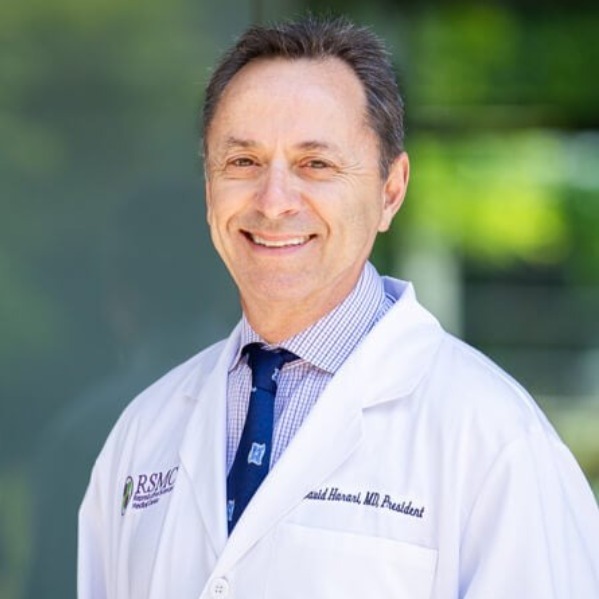
DR. DAVID HARARI
Medical Director of RSMC San Diego
Dr. Harari earned his Medical Doctorate from the University of Georgia Medical Center, completed his internship at the Georgia Medical School, and later finished his residency training at Mercy Medical Center. With over 30 years of clinical experience, Dr. Harari is currently the President of the San Diego Obstetrical and Gynecological Society, which boasts over 400 professional OB-GYN members. Throughout his practice, Dr. Harari deeply respects each patient's personal wishes, providing them with the most professional treatment plans and working collaboratively to help them achieve their goals. He believes in the importance of clear communication and mutual understanding between doctors and patients and is always eager to share his extensive medical experience and offer the best professional advice.
About Dr. David Harari
Other
-
2025/03/13others
Can Vitiligo Be Cured With Reproductive Technology?
-
2025/02/24others
What are the reasons behind failed blastocyst culture?
-
2024/11/06others
How Men Can Face and Prevent Infertility: A Complete Guide



